Why does childhood anxiety matter?

“Because it often doesn’t just go away,” says Dr. Tessa Reardon from the University of Oxford.
Untreated, childhood anxiety can cast a long shadow – affecting everything from education and job prospects, to relationships, health and mental wellbeing well into adulthood.
“And we know it starts young – often as early as five and a half years old,” she adds. “So if we want to make a real difference, we have to start early.”
Since 2020, Reardon has led one of the largest studies ever done on preventing anxiety in children, funded by Kavli Trust. The research tested a simple idea: could a digital support programme for parents stop anxiety disorders from developing in children already showing early signs?
The answer appears to be yes – and cost-effectively, too.
Making help easy to reach
Rather than waiting for parents to seek help – a step many never take – Reardon and her team turned the system on its head.
“We went to them,” she says. “By offering support directly through schools, we made it easy to identify families who might benefit – and to give them help early.”
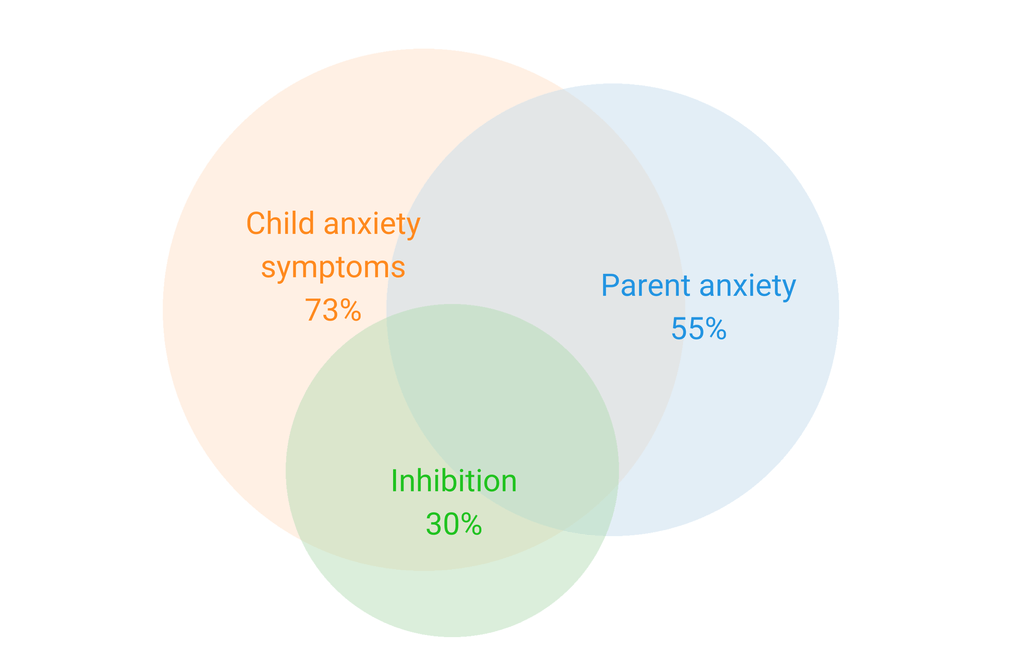
The team used questionnaires filled in by parents to spot common risk factors: shyness, high anxiety in the child or parent.
But they weren’t just casting a wide net.
“We weren’t looking for kids who were just a little worried,” says Reardon. “We aimed to identify those at high risk of developing a clinical anxiety disorder.”
Who took part?
• Children between the age of 4 – 7 years old
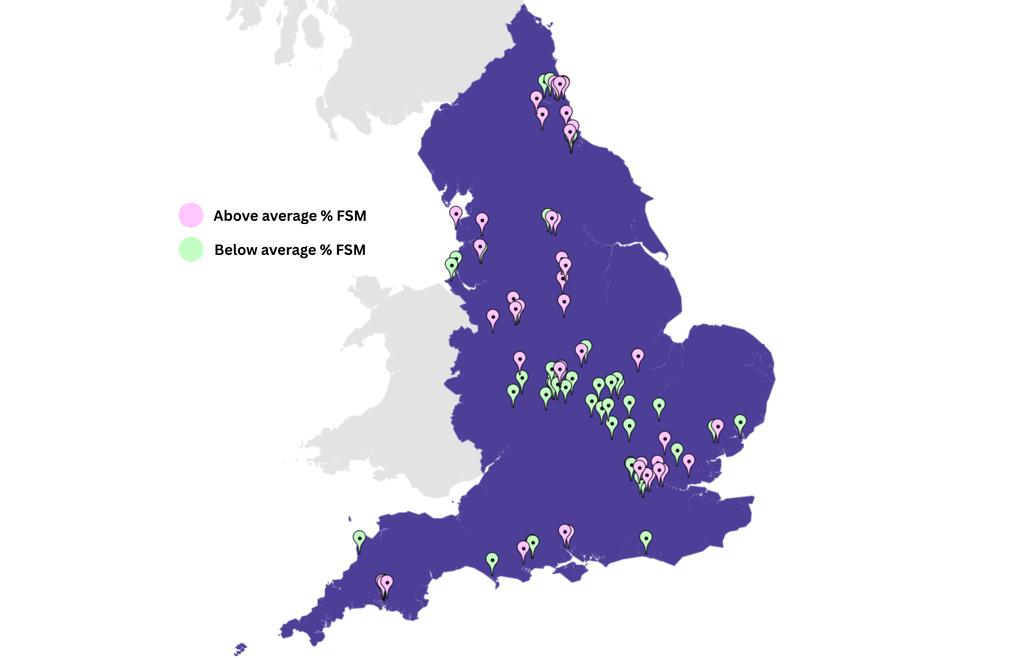
• 95 schools across the UK
• More than 15,000 children with 2000 screened
• Around 1,000 children identified as high-risk
• 75% of parents agreed to take part
Children were randomly placed in one of two groups:
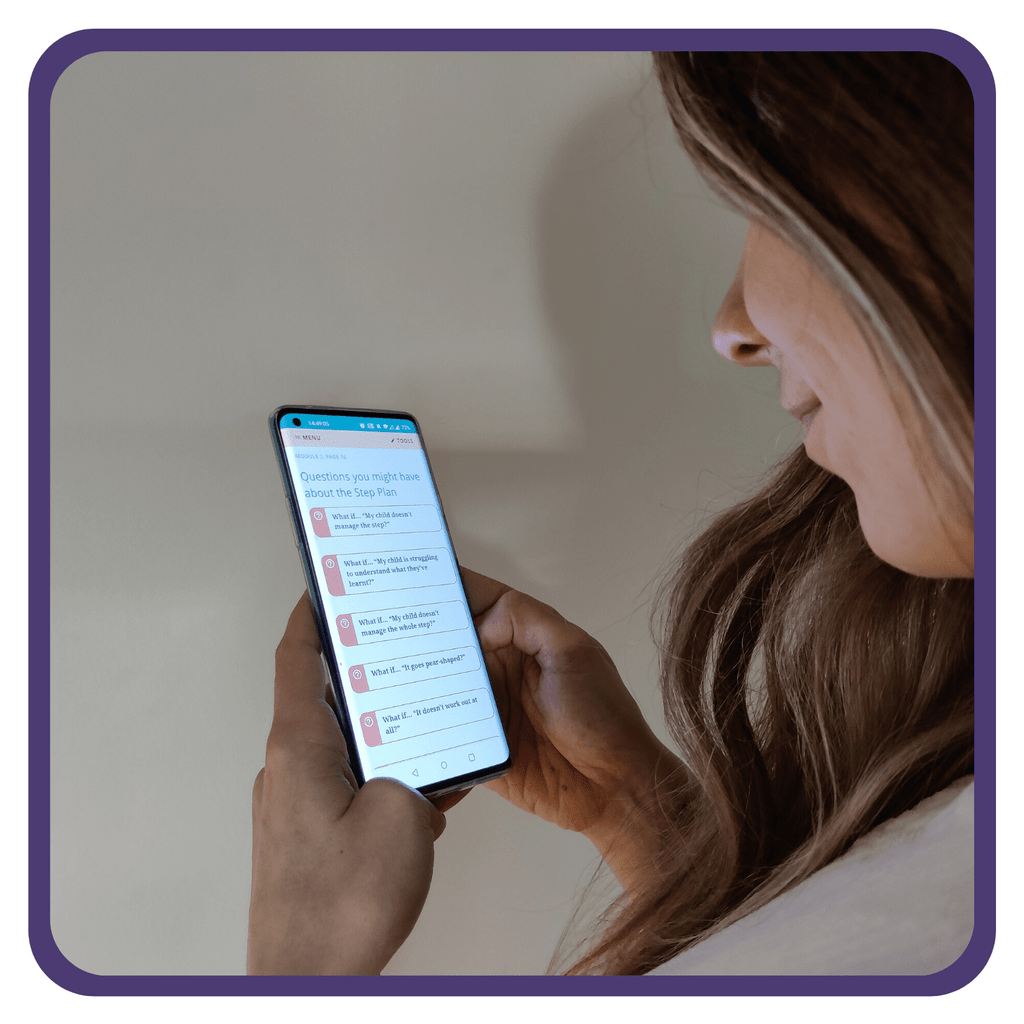
• One received access to a digital parent support programme
• The other received usual school support
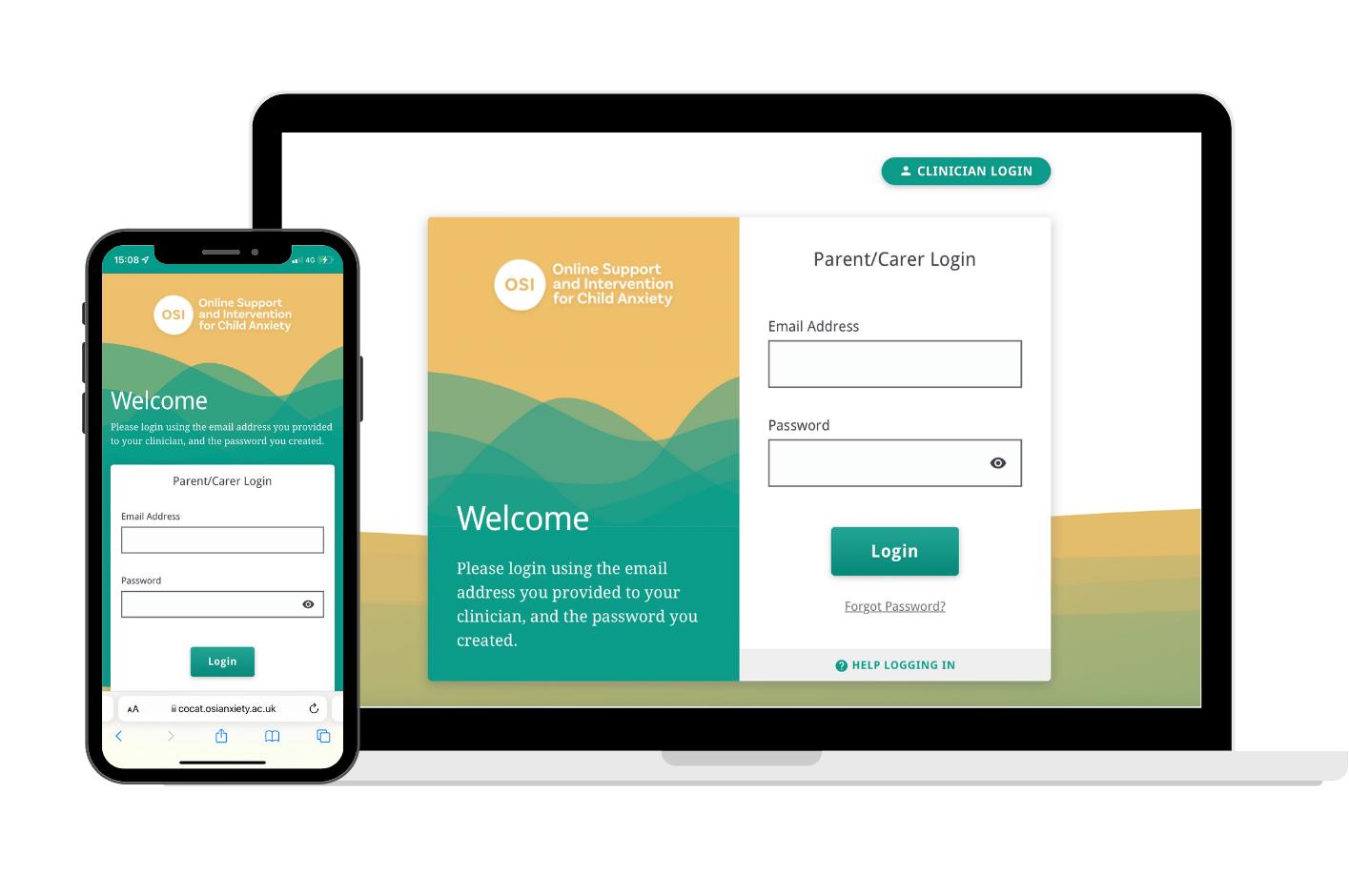
The digital tool used was called OSI – Online Support and Intervention for child anxiety. It’s an online platform designed by mental health professionals to help parents support their child, with therapist guidance and optional mobile app features for the kids.
So… did it work?
It did.
Fewer diagnoses: One year later, only 6.8% of children in the intervention group developed an anxiety disorder, compared to 11.5% in the control group.
Better outcomes: Kids showed fewer symptoms of avoidance and uncertainty. Parents felt more confident helping their child.
Good value for money: Health economists found the programme was well below the NHS’s cost-effectiveness threshold – meaning it offers real bang for the buck.
“This is exactly the kind of evidence policymakers need,” says Reardon. “It shows it works, and it’s worth it.”
Designed for real-world impact
This wasn’t a study done in isolation.
“We designed it with implementation in mind,” Reardon explains. “That was something Kavli Trust really pushed us to think about – not just does it work, but can we use it?”
Now, with fresh funding, Reardon’s team is focusing on rolling the model out across the UK, working with Mental Health Support Teams in schools.
They’re also developing practical tools and training for frontline staff to bring the method into everyday practice.
What’s next?
The team isn’t stopping at anxiety.
“Many of the families in our study were struggling with behavioural issues too,” says Reardon. “So now we’re looking at how to adapt the approach to support a broader range of mental health risks.”
One challenge is making sure disadvantaged families don’t miss out. The study found that participation was lower among families facing social and economic hardship.
“That’s a real problem,” she says. “Social deprivation is a risk factor in itself, so we need to make the tools easier to access for those families.”
Funding applications are already underway to help close that gap.
More than just data
Beyond the numbers, Reardon points to the wider ripple effects of the Kavli Trust-funded project.
“For me personally, this research helped me grow as a scientist and take on work that really matters,” she says.
The project also helped launch the careers of several young researchers – many now pursuing PhDs or training as clinical psychologists.
And the partnerships built with schools during the study are now laying the foundation for a national research and practice network.
The power of open data
Thanks to Kavli Trust’s open-access policy, the rich dataset from the study is now available to other researchers.
“We’re already using it to explore new questions,” Reardon says. “One student is even working on improving how we measure anxiety in children – which is so important. You can’t evaluate impact if you can’t measure it well.”
A model for change
“This is exactly the kind of impact we hope for,” says Ingrid Paasche, General Manager of Kavli Trust. “This study shows how targeted research funding can lead to real change – not just in policy, but in children’s lives.”
Rune Mørland, Head of Strategy and Development, agrees.
“This isn’t just a successful trial,” he says. “It’s a model for early, cost-effective intervention – one that’s already shaping mental health services in the UK.”
The study may be complete, but its influence is just beginning.
ABOUT THE KAVLI TRUST PROGRAMME ON HEALTH RESEARCH
• NOK 172 million allocated to research on child and adolescent mental health from 2017–2024
• Focused on research that leads to real-world benefits for patients, families and healthcare workers
• All projects address specific knowledge gaps identified in collaboration with experts and users
• Final allocation in 2024 – but support for communication and impact continues